Chronic Regional Pain Syndrome (CRPS) is a debilitating condition characterized by intense and persistent pain, often accompanied by changes in skin color, temperature, and swelling. While treatment options for CRPS are limited, one promising approach is the use of Sympathetic Nerve Block. In this article, we will explore the role of the sympathetic nervous system in CRPS, the procedure of Sympathetic Nerve Block, evaluate its efficacy, and discuss the potential risks and complications associated with this treatment option.
Understanding CRPS: An Overview
CRPS, also known as Complex Regional Pain Syndrome, is a complex and debilitating condition that can develop after an injury or trauma, such as a fracture or surgery. It is characterized by chronic and intense pain that is disproportionate to the initial injury. The exact cause of CRPS is not fully understood, but researchers believe it involves abnormal functioning of both the peripheral and central nervous systems.
When an individual experiences an injury, the body’s immune system responds by releasing inflammatory mediators to promote healing. However, in CRPS, there is an exaggerated immune response, leading to widespread inflammation and tissue damage. This abnormal inflammatory response is believed to be a key factor in the development of CRPS.
Furthermore, CRPS is thought to involve changes in the way the nervous system processes pain signals. The nerves become hypersensitive, causing even the slightest touch or movement to be perceived as excruciating pain. This heightened sensitivity to pain is a hallmark characteristic of CRPS.
The Pathophysiology of CRPS
In CRPS, the abnormal immune response triggers a cascade of events that contribute to the development and progression of the condition. Inflammatory mediators, such as cytokines and chemokines, are released and cause widespread inflammation and tissue damage. This inflammation leads to the activation of immune cells, such as macrophages and T-cells, which further perpetuate the inflammatory response.
The inflammatory mediators not only cause tissue damage but also affect blood vessels in the affected area. Blood vessels become leaky, leading to edema (swelling) and changes in skin color and temperature. The affected limb may appear red or purple and feel warmer or colder than the surrounding areas.
Additionally, the abnormal immune response can disrupt the normal functioning of nerves in the affected area. Nerves may become hypersensitive, leading to abnormal pain signaling. This can result in a constant, burning pain that is often described as intolerable. The pain may spread beyond the initial injury site, affecting a larger area of the body.
Symptoms and Diagnosis of CRPS
The symptoms of CRPS can vary from person to person, making diagnosis challenging. However, there are common symptoms that are typically observed in individuals with CRPS. One of the primary symptoms is severe, constant pain that is disproportionate to the initial injury. The pain may be described as burning, throbbing, or shooting.
In addition to pain, individuals with CRPS may experience changes in skin color and temperature. The affected limb may appear mottled, with patches of red, purple, or pale skin. The limb may also feel warmer or colder than the surrounding areas.
Swelling is another common symptom of CRPS. The affected limb may become swollen and puffy, making it difficult to move or use. This swelling is a result of the inflammatory response and increased blood flow to the area.
Furthermore, CRPS can cause changes in hair and nail growth. Hair may become thicker or thinner, and nails may grow faster or slower. These changes are thought to be a result of the disrupted nerve function in the affected area.
Diagnosing CRPS can be challenging as there is no specific test for the condition. It is typically diagnosed based on a thorough evaluation of the patient’s medical history, symptoms, and physical examination. The healthcare provider may also order additional tests, such as X-rays or bone scans, to rule out other possible causes of the symptoms.
Overall, CRPS is a complex condition that involves abnormal immune responses, changes in nerve function, and a wide range of symptoms. It can significantly impact an individual’s quality of life and requires a multidisciplinary approach to management and treatment.
The Role of the Sympathetic Nervous System in CRPS
The sympathetic nervous system plays a crucial role in our body’s response to stress and regulates various functions, including blood flow and pain perception. It is a complex network of nerves that extends throughout the body, working in conjunction with the parasympathetic nervous system to maintain balance and homeostasis.
In CRPS, also known as Complex Regional Pain Syndrome, the sympathetic nervous system becomes hyperactive, contributing to the persistent pain and other symptoms experienced by individuals with the condition. This condition is characterized by intense and debilitating pain, often affecting the limbs, which can be accompanied by changes in skin color, temperature, and texture.
The Sympathetic Nervous System and Pain
Pain signals are transmitted through sensory nerves to the spinal cord and then to the brain. The sympathetic nervous system can modulate these pain signals, either amplifying or dampening the perception of pain. In the case of CRPS, the sympathetic nervous system amplifies pain signals, leading to the severe and constant pain associated with the condition.
When an injury or trauma occurs, the sympathetic nervous system responds by releasing stress hormones, such as adrenaline and noradrenaline. These hormones increase heart rate, blood pressure, and blood flow to prepare the body for a “fight or flight” response. However, in CRPS, this response becomes dysregulated, resulting in a continuous state of heightened sympathetic activity.
Furthermore, the sympathetic nervous system interacts with the immune system, contributing to the inflammatory response observed in CRPS. This inflammation can further sensitize the nerves, leading to increased pain sensitivity and perpetuating the cycle of chronic pain.
How CRPS Affects the Sympathetic Nervous System
CRPS can cause dysfunction of the sympathetic nervous system, leading to abnormal regulation of blood flow, skin temperature, and sweating. These changes can further contribute to the intensity of pain experienced by individuals with CRPS.
One common manifestation of sympathetic dysfunction in CRPS is vasoconstriction, where the blood vessels constrict, reducing blood flow to the affected area. This can result in cold and pale skin, as well as impaired tissue healing. On the other hand, some individuals may experience vasodilation, where the blood vessels dilate, causing redness and warmth in the affected area.
Additionally, abnormal sweating patterns, known as sudomotor dysfunction, can occur in CRPS. Some individuals may experience excessive sweating, while others may have reduced sweating. These changes in sweat production can further contribute to the discomfort and abnormal sensations experienced by individuals with CRPS.
Understanding the role of the sympathetic nervous system in CRPS has led to the development of Sympathetic Nerve Block as a potential treatment option. This procedure involves the injection of an anesthetic medication near the sympathetic ganglia to temporarily block the transmission of pain signals. By interrupting the hyperactivity of the sympathetic nervous system, Sympathetic Nerve Block can provide relief and improve function in individuals with CRPS.
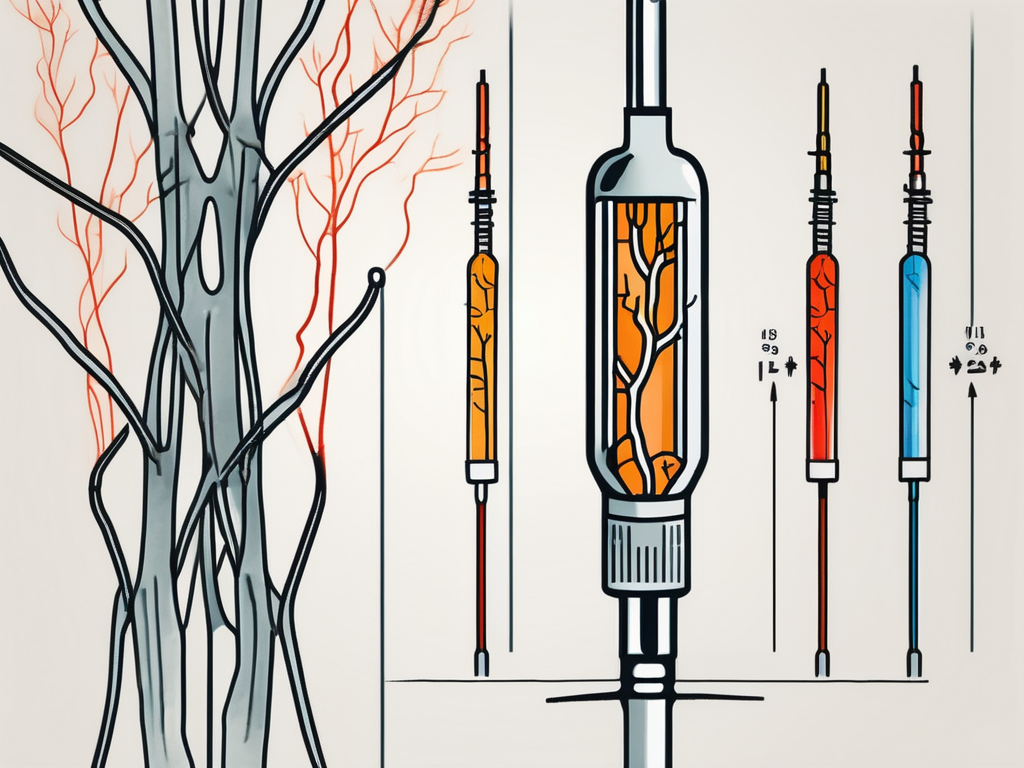
Sympathetic Nerve Block: A Closer Look
Sympathetic Nerve Block is a minimally invasive procedure that involves injecting a local anesthetic into the affected sympathetic nerves. The goal of the procedure is to temporarily interrupt the hyperactivity of the sympathetic nervous system and provide relief from pain and other CRPS symptoms.
The Procedure of Sympathetic Nerve Block
During a Sympathetic Nerve Block, the patient lies on their stomach, and the area to be treated is cleaned and sterilized. A thin needle is then carefully inserted near the affected sympathetic nerves under the guidance of imaging techniques such as fluoroscopy or ultrasound. Once the needle is in place, a local anesthetic is injected to block the transmission of pain signals.
Mechanism of Action: How Does It Work?
The local anesthetic used in a Sympathetic Nerve Block temporarily blocks the transmission of pain signals from the sympathetic nerves to the spinal cord and brain. By interrupting the hyperactivity of the sympathetic nervous system, it can provide pain relief and potentially improve other symptoms of CRPS.
Evaluating the Efficacy of Sympathetic Nerve Block for CRPS
Research studies and clinical trials have shown mixed results regarding the efficacy of Sympathetic Nerve Block for CRPS. While some patients report significant pain relief and improvement in their overall quality of life, others may experience only modest or temporary benefits. The effectiveness of Sympathetic Nerve Block may depend on various factors, including the patient’s individual response to the treatment and the duration and severity of their CRPS symptoms.
Reviewing Clinical Trials and Research Findings
Several clinical trials have been conducted to assess the effectiveness of Sympathetic Nerve Block for CRPS. While some studies have reported positive outcomes, others have found no significant difference between the treatment and control groups. The variability in findings suggests the need for further research to better understand the potential benefits and limitations of this treatment approach.
Patient Outcomes and Quality of Life Post-Treatment
Individual experiences with Sympathetic Nerve Block can vary. Some patients may experience significant pain relief and improvement in their ability to perform daily activities, while others may have a more limited response. It is important for patients considering this treatment option to have realistic expectations and discuss potential outcomes with their healthcare provider.
Potential Risks and Complications of Sympathetic Nerve Block
Like any medical procedure, Sympathetic Nerve Block carries some risks and potential complications. While the procedure is generally considered safe, there is a small risk of infection, bleeding, nerve damage, or an allergic reaction to the local anesthetic. It is important for patients to discuss these risks with their healthcare provider to make an informed decision about the appropriateness of the treatment for their specific situation.
Short-term Side Effects
After a Sympathetic Nerve Block, patients may experience short-term side effects such as temporary numbness or weakness in the affected area, mild pain or bruising at the injection site, or a transient increase in pain before experiencing the full benefits of the procedure. These side effects are usually temporary and resolve on their own.
Long-term Risks and Considerations
There is limited long-term data available regarding the risks and complications associated with Sympathetic Nerve Block for CRPS. It is vital for patients to have an open and honest discussion with their healthcare provider about the potential benefits, risks, and long-term implications of the treatment before making a decision.
In conclusion, Sympathetic Nerve Block holds promise as a treatment option for individuals suffering from CRPS. However, its efficacy and suitability for each patient should be carefully evaluated on a case-by-case basis. It is essential to consult with a knowledgeable healthcare professional to determine the best course of treatment for managing the symptoms of CRPS and to navigate the potential benefits and risks associated with Sympathetic Nerve Block.