Migraine is a complex neurological disorder that affects millions of people worldwide. It is characterized by severe headaches, typically accompanied by symptoms such as nausea, vomiting, and sensitivity to light and sound. While the exact cause of migraine is still not fully understood, recent research has shed light on the role of the sympathetic nervous system in the development and progression of this debilitating condition.
Understanding Migraine: A Brief Overview
Migraine is a chronic condition that impacts the daily lives of individuals who experience it. It is estimated that approximately 1 billion people suffer from migraine globally. Migraine attacks can last anywhere from a few hours to several days and can significantly impair an individual’s ability to function.
Living with migraine is a constant battle, as the symptoms can be debilitating. The pulsating or throbbing pain that accompanies a migraine attack can be excruciating, making it difficult for individuals to carry out their daily activities. In addition to the pain, many people experience visual disturbances, such as seeing flashing lights or blind spots. These visual disturbances can be frightening and add to the overall distress of a migraine attack.
Defining Migraine: Symptoms and Triggers
Migraine is more than just a headache. It is often associated with a range of symptoms, including pulsating or throbbing pain, visual disturbances, and even sensory disturbances. These symptoms can vary from person to person and may be accompanied by additional symptoms such as dizziness, fatigue, and difficulty concentrating.
Identifying the triggers that can lead to a migraine attack is crucial for managing the condition effectively. Hormonal changes, such as those that occur during menstruation or menopause, can trigger migraines in many women. Certain foods, such as aged cheese, chocolate, and red wine, have also been known to provoke migraines in some individuals. Stress, lack of sleep, and environmental factors like bright lights or strong odors can also contribute to the onset of a migraine attack.
Managing migraine triggers can be a complex process, as each person’s triggers can be unique. Keeping a detailed migraine diary can help individuals track their symptoms and identify patterns or triggers. This information can then be used to develop a personalized management plan that includes lifestyle modifications and, if necessary, medication.
The Prevalence of Migraine Worldwide
Migraine affects people of all ages and from all walks of life. It is estimated that approximately 12% of the global population suffers from migraine. Women are three times more likely to experience migraines than men, with hormonal fluctuations playing a significant role in migraine occurrence in women.
The impact of migraine on individuals and society as a whole is significant. The economic burden of migraine is substantial, with substantial healthcare costs, decreased productivity, and increased absenteeism from work or school. Migraine attacks can be unpredictable and can disrupt daily routines, causing individuals to miss out on important events or social engagements. The emotional toll of living with chronic pain and the fear of when the next attack will strike can also take a toll on a person’s mental well-being.
Despite the prevalence and impact of migraine, there is still much to learn about the condition. Ongoing research is focused on understanding the underlying mechanisms of migraine and developing more effective treatments. In the meantime, raising awareness about migraine and providing support for those affected by it is crucial in improving the quality of life for individuals living with this chronic condition.
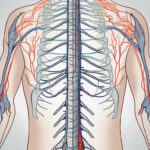
The Sympathetic Nervous System Explained
The sympathetic nervous system is a branch of the autonomic nervous system responsible for the body’s response to stress. It controls the fight-or-flight response, which prepares the body for physical exertion or emergency situations. The sympathetic nervous system regulates various bodily functions, including heart rate, blood pressure, and respiration.
The Role and Function of the Sympathetic Nervous System
The sympathetic nervous system plays a crucial role in maintaining homeostasis and ensuring the body’s survival in challenging situations. When activated, it increases heart rate, constricts blood vessels, and releases adrenaline, preparing the body for physical exertion or stress.
In addition to its immediate responses, the sympathetic nervous system also influences various other bodily functions, such as digestion, immune system modulation, and regulation of body temperature.
How the Sympathetic Nervous System Responds to Stress
Stressful situations trigger the activation of the sympathetic nervous system. When confronted with a perceived threat or danger, the body initiates a series of physiological responses to prepare for fight or flight. These responses include an increase in heart rate and blood pressure, dilation of the pupils, slowed digestion, and increased alertness.
In the context of migraine, stress is considered a significant trigger for migraine attacks. The activation of the sympathetic nervous system during times of stress can potentially contribute to the development and worsening of migraine symptoms.
Furthermore, the sympathetic nervous system is not only responsible for the immediate physical responses to stress, but it also plays a role in long-term adaptations. Chronic stress can lead to an overactive sympathetic nervous system, which can have detrimental effects on overall health. Prolonged activation of the sympathetic nervous system can result in increased blood pressure, heart disease, and a weakened immune system.
Moreover, the sympathetic nervous system’s influence extends beyond the physiological responses to stress. It also affects cognitive functions, such as memory and attention. When the sympathetic nervous system is activated, it can enhance alertness and focus, allowing individuals to respond quickly and effectively to potential threats.
Additionally, the sympathetic nervous system interacts with other systems in the body, such as the endocrine system. When activated, it stimulates the release of stress hormones, including cortisol and adrenaline, which further contribute to the body’s response to stress. These hormones increase energy production, suppress non-essential functions, and promote the mobilization of resources to deal with the perceived threat.
In conclusion, the sympathetic nervous system is a vital component of the body’s stress response. It not only prepares the body for immediate physical action but also influences various other physiological and cognitive functions. Understanding the role and function of the sympathetic nervous system can provide valuable insights into how our bodies adapt and respond to stress, ultimately contributing to our overall well-being.
The Connection Between Migraine and the Sympathetic Nervous System
Recent research has revealed a strong link between migraine and the sympathetic nervous system. During a migraine attack, there is evidence of sympathetic activation, including changes in heart rate variability and peripheral vasoconstriction.
The Physiological Response of the Sympathetic Nervous System to Migraine
Studies have shown that during a migraine attack, sympathetic activation can lead to increased release of norepinephrine, a neurotransmitter that plays a role in pain modulation. It is believed that this increased release of norepinephrine contributes to the heightened pain sensation experienced during a migraine attack.
Furthermore, sympathetic activation may also play a role in the associated symptoms of migraine, such as nausea and vomiting, through its influence on digestive function and motility.
The Impact of Chronic Migraine on Sympathetic Nervous System Function
Individuals with chronic migraine, defined as experiencing migraine attacks on 15 or more days per month, may have altered sympathetic nervous system function. Studies have suggested that chronic migraine may lead to a dysregulation of sympathetic activity, resulting in increased sympathetic tone and reduced parasympathetic activity.
This dysregulation of sympathetic nervous system function may contribute to the persistence and severity of migraine attacks in individuals with chronic migraine.
Moreover, it is important to note that the sympathetic nervous system is not solely responsible for the development and progression of migraines. Other factors, such as genetics, hormonal changes, and environmental triggers, also play a significant role in the onset of migraines.
Genetic studies have identified certain gene mutations that may increase the susceptibility to migraines. These mutations affect various biological processes, including neurotransmitter regulation, ion channel function, and vascular tone. The interplay between these genetic factors and sympathetic nervous system activity may contribute to the complex nature of migraines.
Hormonal changes, particularly fluctuations in estrogen levels, have been linked to migraines in women. Estrogen is known to modulate pain perception and influence the function of the blood vessels in the brain. During certain phases of the menstrual cycle, when estrogen levels are low, women may experience an increased risk of migraines. This hormonal influence, combined with sympathetic nervous system activation, can exacerbate the severity and frequency of migraines.
Environmental triggers, such as stress, sleep disturbances, certain foods, and sensory stimuli, can also activate the sympathetic nervous system and trigger migraines. Stress, in particular, has been shown to increase sympathetic activity and promote the release of stress hormones, which can contribute to the onset of migraines. Identifying and managing these triggers is an essential part of migraine management.
In conclusion, while the connection between migraines and the sympathetic nervous system is well-established, it is crucial to consider the multifactorial nature of migraines. Genetic predisposition, hormonal changes, and environmental triggers all interact with sympathetic nervous system activity to contribute to the development and progression of migraines. Understanding these complex interactions is key to improving the management and treatment of migraines.
Potential Therapies and Interventions
Understanding the impact of migraine on the sympathetic nervous system opens up potential avenues for the development of novel therapies and interventions for migraine management. Both pharmacological and non-pharmacological approaches have shown promise in alleviating migraine symptoms and modulating sympathetic nervous system activity.
When it comes to medications, a variety of options have been developed to target different aspects of migraine pathophysiology, including those that modulate sympathetic activity. One such class of medications is beta-blockers, which are commonly used for hypertension management. Interestingly, these beta-blockers have shown efficacy in preventing migraines by reducing sympathetic outflow. By blocking the effects of adrenaline and noradrenaline, these medications can help calm the overactive sympathetic nervous system, providing relief to those who suffer from migraines.
Another group of medications, known as triptans, work by constricting blood vessels and inhibiting the release of neuropeptides associated with migraine pain. By targeting the physiological mechanisms involved in sympathetic activation during a migraine attack, these medications can provide relief to individuals suffering from migraines. It’s fascinating how these medications can specifically target the intricate processes that occur in the sympathetic nervous system during a migraine episode.
However, it’s not just medications that hold promise in managing migraines. Non-pharmacological interventions have also proven effective in reducing sympathetic nervous system activation and managing migraine symptoms. These interventions can include simple lifestyle modifications, such as stress management techniques, regular exercise, and ensuring adequate sleep. By addressing these lifestyle factors, individuals can help regulate their sympathetic nervous system and potentially reduce the frequency and severity of migraine attacks.
Furthermore, complementary therapies such as acupuncture and biofeedback have shown promise in reducing the frequency and severity of migraine attacks by modulating sympathetic nervous system activity. Acupuncture, an ancient practice originating from traditional Chinese medicine, involves the insertion of thin needles into specific points on the body. This technique is believed to stimulate the body’s natural healing processes and restore balance to the sympathetic nervous system. Similarly, biofeedback techniques allow individuals to gain control over their physiological responses, including sympathetic nervous system activation, through the use of electronic devices that provide real-time feedback. By learning to regulate their sympathetic nervous system, individuals may experience a reduction in the intensity and frequency of migraines.
As research continues to shed light on the intricate relationship between migraines and the sympathetic nervous system, the development of new therapies and interventions holds great promise for those who suffer from this debilitating condition. Whether through medications or non-pharmacological approaches, the goal is to provide relief and improve the quality of life for individuals living with migraines.
Future Research Directions
While significant progress has been made in understanding the connection between migraine and the sympathetic nervous system, there are still many unanswered questions and areas for further research.
Unanswered Questions in the Study of Migraine and the Sympathetic Nervous System
One area of ongoing research is the precise mechanisms through which sympathetic activation contributes to migraine development and progression. Recent studies have suggested that sympathetic nerve fibers release neuropeptides, such as calcitonin gene-related peptide (CGRP), which play a crucial role in the pathophysiology of migraines. However, the exact signaling pathways and interactions between the sympathetic nervous system and CGRP remain to be fully understood.
Additionally, further studies are needed to elucidate the relationship between sympathetic nervous system dysregulation and the transition from episodic to chronic migraine. It is still unclear why some individuals with episodic migraines develop chronic migraines, and whether sympathetic nervous system dysfunction is a causative factor or a consequence of the chronicity.
Furthermore, investigating the potential influence of sex hormones on the interaction between migraine and the sympathetic nervous system could provide valuable insights into the higher prevalence of migraines in women. Estrogen, in particular, has been implicated in modulating the excitability of neurons in the trigeminal system, which is involved in migraine pathogenesis. Understanding the interplay between sex hormones and sympathetic nervous system activity may pave the way for more targeted treatment approaches.
The Potential for New Therapies and Interventions in the Future
The evolving understanding of the complex relationship between migraine and the sympathetic nervous system holds promise for the development of new therapies and interventions. By targeting sympathetic nervous system dysregulation, future treatments may provide more effective relief for individuals suffering from migraines, improving their quality of life and reducing the burden of this chronic condition.
One potential avenue for intervention is the use of neuromodulation techniques to modulate sympathetic nerve activity. Transcutaneous vagus nerve stimulation, for example, has shown promising results in reducing the frequency and severity of migraines by modulating the autonomic nervous system. Further research is needed to optimize the parameters and protocols of such interventions to maximize their efficacy.
Another area of exploration is the development of pharmacological agents that specifically target the sympathetic nervous system. By selectively modulating sympathetic nerve activity without affecting other physiological functions, these drugs could provide more targeted and efficient relief for migraines, minimizing side effects and improving treatment outcomes.
Overall, the future of migraine research lies in unraveling the intricate relationship between the sympathetic nervous system and migraine pathophysiology. By addressing the unanswered questions and exploring new therapeutic avenues, we can hope to alleviate the suffering caused by migraines and improve the lives of millions of individuals affected by this debilitating condition.