The cervical sympathetic nerve plays a crucial role in the functioning of our autonomic nervous system. Understanding the anatomy and functions of this nerve is vital for comprehending its role in various physiological processes. Additionally, awareness of disorders related to the cervical sympathetic nerve and available diagnostic and treatment options can help healthcare professionals provide effective care to patients.
Anatomy of the Cervical Sympathetic Nerve
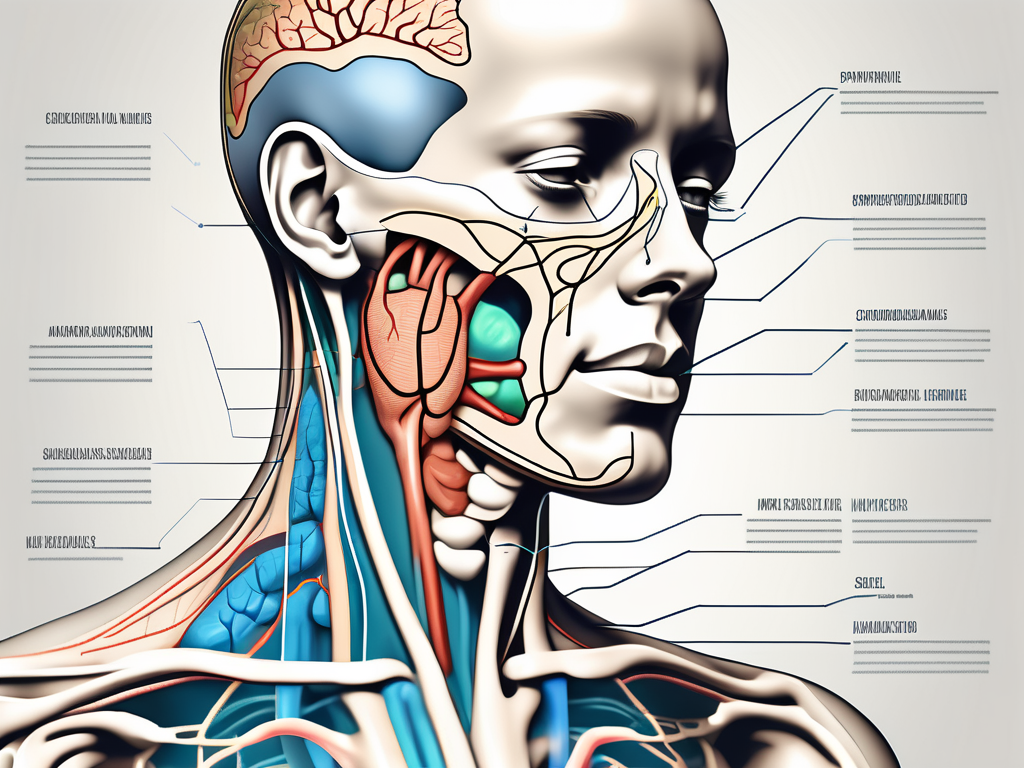
The cervical sympathetic nerve is a crucial component of the sympathetic division of the autonomic nervous system. It originates from the superior cervical ganglion, located at the level of the second cervical vertebra. From there, it extends downwards, forming connections with various structures along its course.
Location and Structure of the Cervical Sympathetic Nerve
The cervical sympathetic nerve runs adjacent to the carotid artery and jugular vein. It consists of a chain of ganglia interconnected by nerve fibers. The nerve fibers pass through these ganglia, allowing communication between different parts of the sympathetic nervous system. This intricate network of connections facilitates the transmission of signals throughout the body.
As the cervical sympathetic nerve courses through the neck, it branches out and forms connections with important structures. One such connection is with the middle cervical ganglion, which plays a role in regulating blood flow to the head and neck. This connection allows for precise control over the blood supply to these regions, ensuring optimal functioning.
Connection to the Autonomic Nervous System
The cervical sympathetic nerve is an integral part of the autonomic nervous system, which regulates involuntary bodily functions. It forms connections with other sympathetic nerves, allowing for coordinated responses to various internal and external stimuli. These connections enable the cervical sympathetic nerve to modulate essential physiological processes such as blood pressure, heart rate, and body temperature.
Furthermore, the cervical sympathetic nerve also connects with the parasympathetic nervous system, which is responsible for the body’s rest and digest response. This connection allows for a delicate balance between the sympathetic and parasympathetic divisions, ensuring that the body can adapt and respond appropriately to different situations. It is through this intricate interplay between the two divisions that the autonomic nervous system maintains homeostasis, keeping the body in a state of equilibrium.
Functions of the Cervical Sympathetic Nerve
Role in Blood Pressure Regulation
The cervical sympathetic nerve plays a crucial role in the regulation of blood pressure. It influences the diameter of blood vessels through a process known as vasoconstriction. By constricting blood vessels, the nerve can increase resistance to blood flow, subsequently raising blood pressure. Conversely, dilation of blood vessels can be achieved through inhibition of the cervical sympathetic nerve, resulting in decreased blood pressure.
When the body is faced with a stressful situation, the cervical sympathetic nerve is activated, leading to vasoconstriction. This response is part of the body’s fight-or-flight mechanism, preparing it for action. By narrowing the blood vessels, the nerve ensures that blood is directed to the vital organs, such as the heart and brain, to meet the increased demand for oxygen and nutrients. This adaptive response helps the body cope with the challenges it faces, ensuring that it can perform at its best.
Impact on Heart Rate
In addition to blood pressure regulation, the cervical sympathetic nerve also impacts heart rate. Stimulation of the nerve can accelerate heart rate, while inhibition can slow it down. This control over heart rate is essential for maintaining cardiovascular health and ensuring optimal circulation.
When the body requires increased oxygen supply, such as during physical exercise, the cervical sympathetic nerve releases neurotransmitters that stimulate the heart to beat faster. This increased heart rate allows for a more efficient delivery of oxygen to the muscles, enabling them to perform at their peak. On the other hand, during periods of rest or relaxation, the inhibition of the cervical sympathetic nerve helps slow down the heart rate, conserving energy and promoting a state of calm.
Influence on Body Temperature
The cervical sympathetic nerve plays a significant role in regulating body temperature. It helps facilitate thermoregulation by controlling blood flow to the skin. By constricting or dilating blood vessels, the nerve can regulate heat loss or retention, allowing the body to maintain its core temperature within a narrow range.
When the body is exposed to cold temperatures, the cervical sympathetic nerve triggers vasoconstriction, reducing blood flow to the skin. This constriction minimizes heat loss from the body’s surface, helping to conserve warmth and maintain a stable internal temperature. Conversely, in hot environments, the nerve promotes vasodilation, increasing blood flow to the skin and facilitating heat dissipation through sweating. This intricate balance of vasoconstriction and vasodilation ensures that the body can adapt to varying external conditions and maintain its temperature homeostasis.
Disorders Related to the Cervical Sympathetic Nerve
Horner’s Syndrome and its Symptoms
Horner’s syndrome is a condition that occurs when the cervical sympathetic nerve is damaged or impaired. This nerve plays a crucial role in controlling various functions in the head and neck region. When it is affected, a cascade of symptoms can arise, causing significant discomfort and inconvenience.
One of the hallmark signs of Horner’s syndrome is the drooping of the eyelid, known as ptosis. This occurs due to the disruption of the sympathetic innervation to the muscles responsible for lifting the eyelid. As a result, the affected individual may experience a noticeable asymmetry in their appearance, which can be distressing.
In addition to ptosis, another common symptom of Horner’s syndrome is reduced pupil size, known as miosis. The pupil, which normally dilates or constricts in response to changes in light, becomes smaller and less responsive on the affected side. This can lead to difficulties in adjusting to varying light conditions, affecting visual acuity and overall visual comfort.
Furthermore, individuals with Horner’s syndrome may also experience decreased sweating on one side of the face, a condition known as anhidrosis. Sweating is an essential mechanism that helps regulate body temperature and maintain optimal thermal balance. When this function is compromised, it can result in discomfort, especially in hot and humid environments.
Diagnosis and treatment of the underlying cause are crucial for managing Horner’s syndrome effectively. Identifying the specific reason for the impairment of the cervical sympathetic nerve is essential in providing targeted therapies and interventions to alleviate the symptoms and improve the overall quality of life for those affected.
Neurological Disorders and their Impact
Certain neurological disorders can affect the functioning of the cervical sympathetic nerve, leading to a wide range of symptoms and complications. Among these conditions, cervical dystonia and autonomic neuropathy are notable examples.
Cervical dystonia, also known as spasmodic torticollis, is a neurological disorder characterized by involuntary contractions of the neck muscles. These abnormal muscle contractions can disrupt the normal flow of nerve signals, including those from the cervical sympathetic nerve. Consequently, individuals with cervical dystonia may experience dysregulation of sympathetic activity, leading to various manifestations.
One of the most common symptoms of disrupted sympathetic activity is abnormal blood pressure. Fluctuations in blood pressure levels can occur, causing episodes of hypertension or hypotension. These fluctuations can have a significant impact on an individual’s overall well-being and may require careful monitoring and management to prevent complications.
Heart rate fluctuations are another potential consequence of disrupted sympathetic activity. The cervical sympathetic nerve plays a crucial role in regulating heart rate, ensuring that it remains within a healthy range. When this regulation is compromised, individuals may experience irregular heart rhythms or palpitations, which can be alarming and may require medical intervention.
Impaired thermoregulation is yet another symptom that can arise from disruptions in sympathetic activity. The cervical sympathetic nerve helps control blood flow to the skin and sweat gland activity, both of which are essential for maintaining optimal body temperature. When these mechanisms are affected, individuals may struggle with temperature regulation, feeling excessively hot or cold even in moderate environments.
Understanding the impact of these neurological disorders on the cervical sympathetic nerve is crucial for developing effective treatment strategies. By addressing the underlying causes and providing targeted interventions, healthcare professionals can help individuals manage their symptoms and improve their overall quality of life.
Diagnostic Procedures for Cervical Sympathetic Nerve Disorders
Physical Examination and Medical History
A thorough physical examination and detailed medical history are essential for diagnosing disorders related to the cervical sympathetic nerve. The healthcare provider will evaluate symptoms, perform neurological tests, and inquire about any underlying conditions or recent injuries that could be contributing factors.
Imaging Tests and their Role
Imaging tests, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, may be utilized to visualize the cervical sympathetic nerve and identify any abnormalities. These non-invasive imaging techniques provide valuable insights into the structure and potential lesions affecting the nerve.
During a physical examination, the healthcare provider may assess the patient’s range of motion in the neck and shoulders, looking for any limitations or discomfort. They may also palpate the neck area, feeling for any swelling, tenderness, or abnormal masses that could indicate a cervical sympathetic nerve disorder. Additionally, the provider may evaluate the patient’s vital signs, such as blood pressure and heart rate, as abnormalities in these measurements can sometimes be associated with nerve dysfunction.
When taking the medical history, the healthcare provider will ask the patient about their symptoms in detail. They will inquire about the nature of the pain or discomfort, its duration, and any factors that may exacerbate or alleviate the symptoms. It is important for the patient to provide accurate and comprehensive information to help the provider make an accurate diagnosis. The provider may also inquire about the patient’s occupation, hobbies, and any recent activities that could have potentially caused or contributed to the nerve disorder.
Treatment Options for Cervical Sympathetic Nerve Disorders
Medication and its Effectiveness
Medication can help manage certain cervical sympathetic nerve disorders. Depending on the underlying condition, medications such as alpha-blockers, beta-blockers, or vasodilators may be prescribed to alleviate symptoms and restore normal sympathetic function. These medications work by targeting specific receptors in the sympathetic nervous system, blocking the action of certain neurotransmitters, or dilating blood vessels to improve blood flow.
Alpha-blockers, for example, work by blocking alpha-adrenergic receptors, which are responsible for constricting blood vessels. By inhibiting this action, alpha-blockers help relax and widen the blood vessels, reducing symptoms such as pain and swelling. Beta-blockers, on the other hand, target beta-adrenergic receptors and help regulate heart rate and blood pressure. Vasodilators, as the name suggests, work by dilating blood vessels, improving blood flow to affected areas and reducing symptoms.
Surgical Interventions and their Outcomes
In severe cases or when conservative treatments fail, surgical interventions may be considered. Procedures such as cervical sympathectomy can be performed to interrupt the sympathetic nerve signals in specific areas. During this procedure, the surgeon carefully identifies and selectively cuts or clamps the sympathetic nerves responsible for the disorder. This interruption of nerve signals can provide relief from symptoms such as excessive sweating, pain, or abnormal blood flow.
While surgical interventions can be effective, they are not without risks. Complications such as infection, bleeding, or damage to surrounding structures may occur. Additionally, the outcomes of these procedures can vary depending on the individual and the specific disorder being treated. Some patients may experience significant relief from symptoms, while others may only see a partial improvement. Close post-operative monitoring and follow-up care are crucial to ensure optimal outcomes and manage any potential complications.
The Future of Cervical Sympathetic Nerve Research
Advances in Treatment Techniques
Ongoing research in the field of cervical sympathetic nerve disorders aims to refine existing treatment techniques and explore new avenues for intervention. Advances in technology, such as minimally invasive surgical approaches and targeted drug delivery systems, show promise in improving patient outcomes and reducing potential complications.
One area of focus in treatment advancements is the development of novel therapies that specifically target the cervical sympathetic nerve. Researchers are investigating the use of neurostimulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and pulsed radiofrequency ablation, to modulate the activity of the nerve and alleviate symptoms. These techniques have shown promising results in early studies, offering a non-invasive alternative to more invasive procedures.
Potential for New Diagnostic Tools
In addition to treatment advancements, researchers are also focused on developing new diagnostic tools for cervical sympathetic nerve disorders. Enhanced imaging techniques, such as functional MRI and neurophysiological testing, may provide more detailed information about nerve function and aid in the early detection of abnormalities.
Another area of interest in diagnostic advancements is the exploration of biomarkers that can indicate the presence or progression of cervical sympathetic nerve disorders. By identifying specific molecules or genetic markers associated with these conditions, healthcare professionals may be able to diagnose and monitor patients more effectively, leading to earlier intervention and improved outcomes.
Furthermore, researchers are investigating the potential of artificial intelligence (AI) algorithms in analyzing complex data sets obtained from diagnostic tests. By leveraging machine learning techniques, AI systems can identify patterns and correlations that may not be readily apparent to human observers, enhancing the accuracy and efficiency of diagnosis.
In conclusion, a comprehensive understanding of the cervical sympathetic nerve is essential for healthcare professionals involved in the assessment and management of related disorders. From its anatomy and connection to the autonomic nervous system to its role in blood pressure regulation, heart rate, and body temperature, this nerve plays a vital role in maintaining homeostasis. With continued research and advancements in diagnostic and treatment options, healthcare providers can improve patient outcomes and enhance our understanding of the intricate functions of the cervical sympathetic nerve.